Scepticism from doctors following manifesto launches
of Fellows & members not confident
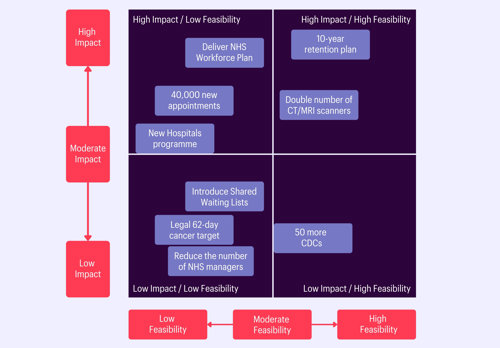
The survey tested nine policies from the Liberal Democrat, Conservative and Labour manifestos which we deemed significant, we did not test all manifesto health policies.[1] It asked about both the extent to which the policies might improve patient care and the how feasible they would be to implement. We did so without attributing any of the policies to the parties which proposed them.
The matrix to the left sorts the policies tested with RCR Fellows and members into a visual for how they have been perceived in terms of feasibility and impact on patient care.
The nine policies captured a range of subjects which could impact the work of our specialities and the wider NHS and included some policies on which there is cross party agreement. The response of our insight panel shows that while there are some policies which respondents feel are feasible, there is a general sense that many of the policies are not. There was also quite a range of opinions on the potential impact of these policies, which can be generally categorised using the matrix above compared with their perceived feasibility to be implemented.
The policies seen as most likely to improve patient care:
said a 10-year retention strategy was likely to improve patient care
said the Long Term Workforce Plan was likely to improve patient care
felt an additional 40,000 appointments, scans and operations each week would be positive
Retention:
79% of our survey respondents said that a 10-year retention strategy, as proposed in the Liberal Democrat manifesto, was likely to improve patient care. This is the policy about which most respondents were positive and one of the only policies which they felt was also feasible for the next government to deliver. When asked what one policy would improve clinical oncology and clinical radiology in the NHS, staff retention was mentioned most frequently.
Given the importance of retention, the RCR welcomes the Liberal Democrat’s ambitions to put retention front and centre of their NHS pledges. The devil would, however, be in the detail, particularly what retention measures would be prioritised. Retention is a key part of the RCR’s three-point plan for supporting the clinical radiology and clinical oncology workforce. We believe that the next government should work to keep the vital skills and experience of doctors in the system through introducing basic support measures, including but not limited to up-to-date computer hardware and sufficient administrative support, as well as offering more flexible working patterns as default. Such measures should be set out in the next iteration of the NHS Long Term Workforce Plan (LTWP), which despite containing a commitment to improve retention, is critically lacking in detail on this topic.
Workforce planning and recruitment:
The Long Term Workforce Plan also includes measures to increase recruitment into the NHS, and all three main parties in England put commitments to the LTWP in their manifestos. Commitment to delivering the LTWP was one of the policies about which our survey respondents were most positive, with 69% saying that it was likely to improve patient care. The fact that the two policies ranked as the most likely to impact patient care were related to supporting workforce capacity once again shows its importance to our Fellows and Members. However, respondents were less positive about the feasibility of implementing the LTWP than some other policies with only 43% of respondents saying they thought it is feasible, suggesting that there is recognition of the challenge of implementing such a plan.
We are acutely aware of the importance of the LTWP for the NHS, which was long overdue in its publication. For the plan to be successful, it should be fully funded and updated regularly to reflect changing realities in our system. The next government should commit to future iterations of the plan, and these should include more detail on speciality training, with commensurate increases in foundation and speciality training places to match those increases in undergraduate places.
40,000 appointments:
Labour’s policy to have an additional 40,000 appointments, scans and operations each week was one which 55% of respondents felt would have a positive impact on patients. However, less than 1 in 5 (18%) of respondents believe that the next government would be able to implement it.
While in theory this seems like a sensible approach to reducing waiting lists, we are keen to understand how staff will be encouraged to commit to extra hours on top of their already incredibly arduous workloads without threatening further burnout amongst NHS staff.
Doubling the number of scanners:
Doubling the number of MRI and CT scanners is another flagship Labour policy which respondents believed could improve patient care. It was one of just three policies which respondents felt was generally more feasible to deliver than not.
The RCR has previously welcomed this investment.[2] The NHS has too few scanners and many of those it currently has are seriously outdated. We also welcome the boost in funding for this policy, which has now increased from the £171 million first proposed to £250 million per year - which is in line with RCR estimates, privately shared with Labour, for the cost of doubling the number of scanners.
If this policy is to be effective at improving patient care, there are a number of things a Labour government would need to consider. These include the location of new machines and the costs of building work required to install them. Most importantly, Labour would need to consider how these machines will be staffed and how the extra scans generated would be reported.
“There is no point buying more scanners if there’s no one to report the scans”.
An insight panel member
New hospitals:
Both Labour and the Conservatives committed in their manifestos to the New Hospitals Programme. While generally members believe this would improve patient care, almost two thirds (64%) of respondents think that it’s unfeasible for the next government to implement.
Questions remain around this policy, particularly regarding its timelines. The House of Commons Public Accounts Committee concluded that the 2030 target set by the Conservatives was unrealistic. [3] The next government will need to consider the level of funding required to fulfil this commitment, and how new hospitals will be staffed and equipped.
More feasible, but will it improve patient care?
Community Diagnostic Centres
While almost half of survey respondents (49%) felt that the Conservative manifesto commitment to open a further 50 Community Diagnostic Centres (CDCs) was feasible, only 43% said that it was likely to improve patient care.
The CDC programme has to date been successful in expanding diagnostic capacity. The RCR advocates for CDCs to be located in the areas of greatest need and for ensuring that they are easily accessible to their local communities.
For this policy to have the greatest impact, the next government should consider the staffing of CDCs, ensuring that they can be operated without any negative impact on local acute sites and that investment in the workforce is in line with the increasing number of scans resulting from CDC expansion. We would also call on the Conservatives to be clear about whether these are 50 entirely new CDCs or whether these are 50 CDCs being transferred from temporary to permanent capacity, given that at least that number of the 160 sites currently open are temporary.
Policies seen as unfeasible and unlikely to impact patients
Shared waiting lists:
Only 43% of our respondents felt that using shared waiting lists and pooled resources to reduce waiting times would improve patient care, while 33% said that it was unfeasible to deliver.
The RCR sees some potential in using this method to address the backlog, but only if done with careful planning to ensure that the workforce and equipment capacity exists. There is an opportunity here to address gaps in regional provision of speciality services such as interventional radiology and acute oncology. However, there is limited spare capacity across the whole system, so it is uncertain to what extent this policy would shift the dial. If nobody has spare capacity to share, then pooling resources will only make a marginal impact on waiting lists. We would like to see the next government engage closely with local clinical leaders to ensure that there is enough capacity locally for this to work, and work with them to shape how this policy would function on the ground.
62-day cancer target:
A key line from the Liberal Democrats throughout the election campaign has been about introducing a new “legal right” for all patients to start treatment within 62-days of an urgent referral, with the aim of boosting cancer survival rates. Insight panel respondents felt that this policy was unlikely to improve patient care and were also doubtful about the feasibility of this being implemented.
It is also unclear how this policy would result in improvements to waiting times performance and patient outcomes without significant investment in the workforce. Simply making a target law will not change the facts on the ground. We are also unclear on the consequences of not achieving these targets for trusts/health boards. In the current environment, the effectiveness of disciplinary action would be questionable.
Reducing the number of NHS Managers:
The Conservative Manifesto commits them to “cut waste and bureaucracy in the NHS” by reducing the number of managers by 5,500, which they claim would release £550 million for frontline services. This policy is one which the insight panel felt would neither improve patient care nor be feasible to implement.
Implementing a policy which reduces managers in an already under-managed NHS is ill-thought through.[4] All party manifestos have been clear on the scale of the challenge facing the NHS. They are all ambitious in their plans for implementing new technology, systems and innovations to support patients and ensure that they are seen in a safe and timely manner. Reducing the number of managers, who would be responsible for overseeing these large-scale innovation projects and ambitious plans to boost NHS productivity, could have a negative impact on the ability of the NHS to deliver on these plans.
Conclusions:
RCR Fellows and Members who contributed to the Insight Panel have given us a firm foundation with which to engage with all parities on their priorities and promises for the NHS. They have shown that, that while some policies may improve patient care, there will be significant challenges to implementing them for any future government.
When asked what one policy would improve clinical radiology and clinical oncology in the NHS Fellows and Members echoed what we have heard for many years now. Workforce, specifically increasing speciality training places and retaining more staff, is the most important thing for the next government to prioritise. Investment in the workforce is central to the workability of all other policies. Further investment in scanners, IT and equipment was also high on our members’ list of priorities.
The lack of confidence among our Fellows and members in the ability of the future government to improve radiology and oncology services is stark.
The next government has a unique opportunity to shift from crisis management to transformative change, securing the future health of the UK. Addressing workforce shortages, expanding diagnostic capacity, and enhancing infrastructure are crucial steps towards this goal. We are committed to working with the next government to achieve these much-needed transformations, and to keep our Fellows and Members updated on our work to influence policy.
“The general election presents a moment for reflection as parties of all political colours put forward their ideas for how the NHS should be supported. The manifestos, however, offer solutions to short term problems, not long-term solutions to the big challenges we face. They look to treat the symptoms, but not the cause. The cure for the NHS’s biggest challenges is a workforce plan that puts staffing on a sustainable footing, coupled with increased investment in capital to deliver technological innovations that would transform how we do healthcare.
A large number of colleagues indicated in the survey that they lacked confidence in whoever forms the next government to improve clinical radiology and clinical oncology services. Politicians have work to do if they are to persuade us that we can work together to transform healthcare.
I am grateful, as always, to the Fellows and Members who took time out of their busy schedules to support our work by filling out this Insight Panel.”
Dr Katharine HallidayPresident of The Royal College of Radiologists
Insight Panel data
How likely are the following policies to improve patient care? (142 respondents)
|
|
Very Unlikely |
Unlikely |
Neither Unlikely nor Likely |
Likely |
Very Likely |
Don’t Know |
|
A legal right for all patients will start treatment within 62-days of an urgent referral |
11% |
27% |
26% |
24% |
9% |
2% |
|
Deliver the new hospitals programme with 40 new and refurbished hospitals |
13% |
12% |
23% |
39% |
11% |
3% |
|
40,000 more operations, scans and appointments each week |
6% |
18% |
16% |
46% |
9% |
5% |
|
Build 50 more Community Diagnostic Centres |
14% |
19% |
23% |
32% |
11% |
1% |
|
Introduce shared waiting lists and pool resources across nearby hospitals to allow patients to be treated quicker |
11% |
25% |
20% |
34% |
9% |
2% |
|
Retain more staff across the NHS through a 10-year retention plan |
4% |
10% |
6% |
37% |
42% |
2% |
|
Double the number of NHS CT and MRI scanners |
11% |
18% |
18% |
37% |
15% |
1% |
|
Deliver the NHS Long-Term Workforce plan to train the staff we need |
6% |
10% |
11% |
32% |
37% |
4% |
|
Reduce the number of NHS managers by 5,500 to spend more on frontline services |
15% |
25% |
19% |
23% |
16% |
2% |
How feasible would it be for the next government to implement these policies? (141 respondents)
|
|
Very Unfeasible |
Unfeasible |
Neither Unfeasible nor feasible |
Feasible |
Very Feasible |
Don’t Know |
|
A legal right for all patients will start treatment within 62-days of an urgent referral |
18% |
31% |
21% |
19% |
7% |
4% |
|
Deliver the new hospitals programme with 40 new and refurbished hospitals |
23% |
40% |
13% |
23% |
1% |
1% |
|
40,000 more operations, scans and appointments each week |
27% |
35% |
16% |
17% |
1% |
3% |
|
Build 50 more Community Diagnostic Centres |
14% |
19% |
17% |
45% |
4% |
1% |
|
Introduce shared waiting lists and pool resources across nearby hospitals to allow patients to be treated quicker |
12% |
18% |
23% |
38% |
7% |
3% |
|
Retain more staff across the NHS through a 10-year retention plan |
9% |
22% |
15% |
43% |
10% |
1% |
|
Double the number of NHS CT and MRI scanners |
10% |
26% |
12% |
45% |
6% |
1% |
|
Deliver the NHS Long-Term Workforce plan to train the staff we need |
11% |
28% |
16% |
40% |
3% |
3% |
|
Reduce the number of NHS managers by 5,500 to spend more on frontline services |
11% |
27% |
23% |
30% |
6% |
3% |
How confident are you that whoever forms the next government will improve clinical radiology and clinical oncology in the NHS? (141 respondents)
|
Extremely confident |
0% |
|
Very confident |
0% |
|
Somewhat confident |
11% |
|
Not so confident |
37% |
|
Not at all confident |
48% |
|
Unsure |
4% |
References
[1] The three largest parties in England in the last parliament. Looking at England as health is a devolved matter.
[2] RCR, RCR response to Labour’s ‘Fit For The Future Fund’ (9 Oct 2023). Available at: https://www.rcr.ac.uk/news-policy/latest-updates/rcr-response-to-labour-s-fit-for-the-future-fund/
[3] House of Commons, Public Account Committee The New Hospitals Programme (17 November 2023) Available at: https://publications.parliament.uk/pa/cm5804/cmselect/cmpubacc/77/report.html
[4] NHS Confederation, Are there too many NHS Managers, Available at: Are there too many NHS managers? | NHS Confederation