Upcoming changes to the CR2B
Background
The changes detailed below will be implemented to the CR2B exam from June 2025 onwards. These changes are being introduced to ensure that the exam reflects current practice and GMC standards for assessment. The aim of the changes is to ensure the exam remains a fair and robust way to assess the knowledge and skills required across the curriculum at the expected level of competence.
It is important to know that some core elements of the exam will remain the same:
- Three exam components (an Oral component and two reporting components) make up CR2B.
- All components are to be taken at the same sitting.
- The type and level of content included in the exam is unchanged.
Details of what will remain the same and what will change for each exam component are listed below.
Oral component
The Oral component will continue to be delivered across two sessions, each of 30 minutes duration and each with a pair of examiners presenting cases to the candidates. Candidates will still be required to attend an exam venue and the Oral will be delivered via video link with the examiners.
Examiners will present cases using a range of imaging modalities. Candidates will have the ability to manipulate and scroll through images.
The level and type of content used within the Oral component will remain the same.
A logical and informed approach to image interpretation, as well as a clear ability to debate the merits, relevance and role of techniques that might assist in further investigation of diagnostic problems, will be expected. Examiners may ask supplementary questions to further assess a candidate’s understanding of the problem.
The following changes will be introduced:
- Changes to the system of scoring with the use of a domain-based marking approach and a new standard setting methodology.
- Increased standardisation of the exam. There is a central bank of Oral cases and candidates will be presented with a set of cases that have been quality reviewed. The set of cases will be balanced across the syllabus and for difficulty. All candidates will encounter the same number of cases (six cases per Oral session, 12 cases in total)
- Candidates can expect cases of varying difficulty (some being expected to be relatively easy and some harder). This is accounted for in marking and standard setting.
- All candidates being examined on the same day will be presented with the same set of cases. To support this, candidate quarantine will be introduced. This means a period of waiting before/after the Oral sessions in a designated waiting area. Arrival and departure times will be indicated to candidates on their timetables. This step is important to ensure that the exam security is maintained
- The delivery of the exam will move to the Risr/Assess platform. This platform will support the video link between examiners and candidates and the sharing of cases with the candidate. This is the same platform currently used for the CR2B reporting components
Reporting components
The two separate reporting components will continue to be delivered on the same day. Candidates will still be required to attend an exam venue and both components will remain delivered via the Risr/Assess platform.
Across the reporting components, there are no fixed criteria for coverage of specific pathology, but content will be appropriately balanced and representative. The cases may vary in complexity and difficulty – this will be accounted for in standard setting.
Long case reporting
There is no change to the format, exam structure, or content of this component. It will continue to be six cases, each of which requires a report. Each case may comprise multiple modalities and sequences. Brief case histories and other relevant clinical data for each case are provided.
Candidates responses are recorded in a standard format:
- Observations: observations from all the imaging studies available, including relevant positive and negative findings.
- Interpretation: interpretations of the observed findings; for example, describing whether the mass or process observed is benign, malignant or infective rather than neoplastic, giving reasons.
- Main or Principal Diagnosis: A single diagnosis based on the interpretations. If a single diagnosis is not possible, then the most likely diagnosis should be stated.
- Any Differential Diagnoses: For some cases there will be no differential diagnoses; in others a few may merit inclusion. These should be limited in number and brief, and the report should indicate why these were less likely than the main or principal diagnosis above.
- Any Relevant Further Investigations or Management: Any further appropriate investigations or clinical management.
The following will be introduced:
- Changes to the scoring system and standard setting
Short case reporting
This new assessment will replace the current rapid reporting component. This new component does not represent a fundamental change in what is assessed i.e. it remains primarily intended to assess interpretation of plain radiographs. The new question format will allow for more complex imaging to be used – but still appropriate to the level of the exam. The format will be as follows:
- A short answer question type. Candidates will be presented with a case which will include a brief clinical history and plain radiograph. Candidates will be asked to write a short report and include their next recommended management step for the patient.
- There will be 25 questions in the component, and a two-hour duration.
- A new scoring system to align with the question format and use of standard setting will be used.
- The component will not include cases where the images would be considered as ‘normal’.
The coverage of chest, musculoskeletal and abdominal X-rays will fall approximately within the ranges indicated below:
- CXR: 50-60% of the set
- MSK: 40-50% of the set
- AXR: up to 4% (1 question) of the set
The coverage of adult and paediatric cases will be split as indicated below:
- Adult cases: approximately 75%
- Paediatric cases: approximately 25%
Short case reporting sample questions
Sample short cases and sample answers are provided below to give guidance on what constitutes a good, average and poor answer. Short, simple statements of your observations, diagnosis and recommendation are all that is needed. You do not need to write full sentences.
The examiner marking guidance shown next to the sample answers is intended to give context on the marking of each case. The examiner marking guidance indicates key findings, diagnosis and recommended onward management to help to explain why a particular answer would score more than another. Examiners will use the mark scheme descriptors (as detailed in the scoring system) alongside this marking guidance to score candidates’ responses and each case will be awarded a score of 0 – 5. There is no concept of a pass or fail per case as all cases are standard set as to their difficulty. The modified Angoff process is used to determine the pass mark for each sitting based on the content used.
Please note that the examiner marking guidance will not be available to candidates as part of their results/feedback. For further information on the short case scoring please see the link to scoring system info/marking descriptors on our website June 2025 FRCR Part 2B (Radiology) - CR2B scoring system | The Royal College of Radiologists
Age 14, male. Referral from ED. History: Painful wrist after falling off skateboard.

| Sample answer | Answer type | Examiner marking guidance |
|
Distal radius fracture through the growth plate, with dorsal displacement. |
Good |
Age 14, male. Referral from ED. History: Painful wrist after falling off skateboard. Findings: Management: |
|
There is a displaced fracture of the distal radius with dorsal displacement (Colles type fracture). |
Average |
|
|
Left radiocarpal dislocation |
Poor |
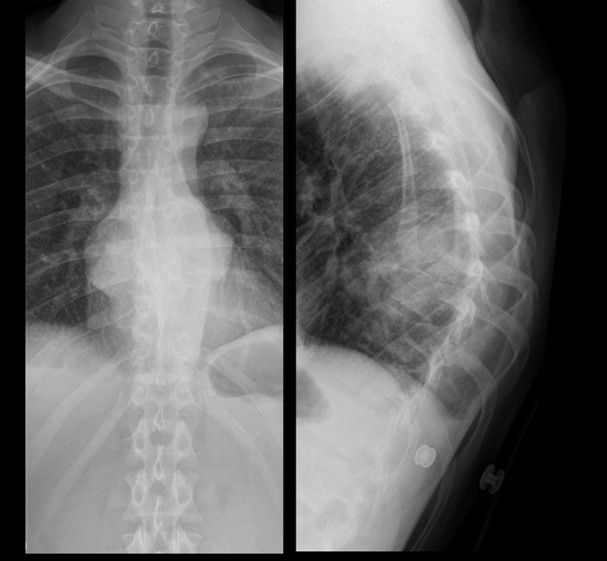
Age 81 male. Referral from GP. History: Cough and weight loss

| Sample answer | Answer type | Examiner marking guidance |
|
Triangular opacity projected over the left heart with obscuration of the medial left hemidiaphragm and loss of volume of the left hemithorax. Increased density noted at the left hilum. Appearances are in keeping with left lower lobe collapse. Causes include central obstructing tumour and mucus plugging. Lungs show multiple confluent opacities some showing appearance in keeping with pleural plaques (I would compare with previous studies). There is prominent right paratracheal soft tissue. Urgent CT chest and upper abdomen to further investigate. |
Good |
Age 81 male. Referral from GP. History: Cough and weight loss Findings: |
|
Left lower lobe collapse with volume loss CT thorax, abdomen and pelvis for further evaluation and staging |
Average |
|
|
Right upper zone mediastinal mass medially likely posterior mediastinum, apical/parenchymal mass cannot be excluded. Bilateral ill-defined patchy focal lesions and reticular opacities. |
Poor |
Age 18 female. Referral from GP. History: painful left knee

| Sample answer | Answer type | Examiner marking guidance |
|
There is an osteochondral defect in the lateral aspect of the medial femoral condyle. There is a bone fragment centrally within the joint space. No joint effusion. Knee MRI and Orthopaedic referral |
Good |
Age 18 female. Referral from GP. History: painful left knee Findings:
|
|
There is lucency projected over the lateral femoral condyle of left femur in keeping with an osteochondral defect. A cortical fragment seen in the intercondylar space. No large knee joint effusion identified. Normal alignment Orthopaedic referral and further assessment with MRI may prove beneficial. |
Average |
|
|
Well-defined lesion in the right distal femur, with sclerotic margins and a narrow zone of transition. No periosteal bone formation. Referral to orthopaedics due to pain. No concerning imaging features so no further investigation needed. |
Poor |
Age 31 male. Referral from ED. History: Post assault

| Sample answer | Answer type | Examiner marking guidance |
|
Right angle of the mandible fracture Refer to max fax surgeon for further management |
Age 31 male. Referral from ED. History: Post assault
Findings: |
|
|
Acute fracture of the right mandibular angle Formal OPG/mandibular views to assess for further fracture. |
Average |
|
|
Left inferior orbital rim fracture Referral to maxillofacial surgeons |
Poor |
New-born male. Referral from NNU. History: traumatic birth due to shoulder dystocia, query clavicular fracture.

| Sample answer | Answer type | Examiner marking guidance |
|
-Nasogastric tube passes into stomach, tip not visualised. Urgently phone NNU to ensure findings are known.
|
Good |
New-born male. Referral from NNU. History: traumatic birth due to shoulder dystocia, query clavicular fracture Findings: |
|
Patient rotated to the left. Notify NICU team.
|
Average |
|
|
NGT in situ appears satisfactory. no clavicle fracture or dislocation seen. imaged lungs appear normal. No further management |
Poor |
Age 24 male. Referral from GP. History: increasing back pain
| Sample answer | Answer type | Examiner marking guidance |
|
Bilateral paravertebral stripe widening at T8 with collapse of T8 vertebral body and kyphosis. Urgent MRI whole spine with contrast. Inform referrer urgently. Antibiotics. Microbiology. Drainage. |
Good |
Age 24 male. Referral from GP. History: increasing back pain Findings: |
|
Soft tissue mass in the posterior mediastinum causing complete collapse and destruction of a mid-thoracic vertebra and focal kyphosis, this is concerning for spondylodiscitis Compare to previous CXR, email GP the report, advise urgent MRI spine for further evaluation |
Average |
|
|
-Paravertebral soft tissue densities projected in the retrocardiac region bilaterally. This corresponds with density projected over vertebral bodies on the lateral projection Imp: Paravertebral masses - likely neurogenic e.g. Neurofibroma, schwannoma MRI Thorax is advised. |
Poor |
CR2B pass/fail decisions
The current overall CR2B structure will be maintained whereby all components are taken at the same sitting. However, there will be an adjusted method of calculation to identify pass/fails.
For further information see the scoring system information page.
Introduction to changes to the FRCR 2B Exam
FAQs
This change was initiated by the RCR to ensure that we can maintain and demonstrate to our regulator that we have a high quality, fair exam whilst supporting an increase in capacity. It also ensures that the exam stays relevant to the needs of the curriculum and training programmes.
We had expert psychometric advice provided to the project team and regular consultation with training programme directors, heads of school and trainees via the RCR’s Junior Radiologist Forum. We had further input from trainees (specifically feedback from piloting exercises) and current examiners (following piloting, standard setting trials, re-marking exercises).
All RCR exams must meet rigorous standards set out by the General Medical Council (GMC). The changes have been thoroughly reviewed by the GMC and were granted approval in November 2024.
The curriculum being examined, and the level of competence expected, is not changing, so you should prepare and revise your radiological knowledge and skills in the same way as before the change. You should make use of the guidance and resources on the RCR website to ensure you are ready for the format and delivery methods.
Instructional videos and updated exam content on the risr/Assess demonstration site will be available soon.
The RCR will be using the same exam venues as in recent years.
On each day of the Oral component, all candidates will be examined on the same set of cases. To ensure that nobody has an unfair advantage by being told about the cases in advance, we must keep candidates isolated.
Exam venues will have rooms set aside for candidates to wait before and after taking the Oral component. Whilst quarantine times may vary, all candidates should be prepared to spend most of the day at the venue. Quarantine times will be indicated on candidates’ individual timetables.
You will not be allowed to use electronic devices whilst being quarantined. Paper-based reading material (such as books, printed text or handwritten notes) is allowed. Candidates suspected of breaking quarantine rules will be investigated in line with the RCR’s Exam Misconduct Policy.
The changes introduced to the scoring system ensure that the exam is fair and appropriately discriminates between passing and failing candidates. They should not make any difference to the way you prepare for the exam or answer questions.
The risr/Assess platform (previously called Practique) has been used for some years for the Rapid Reporting and Long Case components and we are happy that the image definition and manipulation features are sufficient for allowing a fair assessment of candidates’ abilities. We have conducted pilots using the new platform for delivery of the Oral component and it has performed well. Image quality checks will be performed ahead of each sitting as part of the exam's routine quality assurance processes.
The new Short Cases are replacing the old Rapid Reporting as the latter does not reflect current radiological practice. Plain radiographic interpretation is an essential skill for radiologists, particularly in the areas of paediatric imaging and chest imaging where the plain radiograph is likely to remain a key imaging modality for the foreseeable future. The Short Case component will not only assess a candidate’s ability to interpret plain radiographs but also their skill in writing accurate and concise reports with appropriate recommendations to the referrer on further imaging or management, allowing for a more in-depth assessment of plain radiographic interpretation skills. We believe it will be a more authentic examination as candidates will now be provided with clinical/patient information for each case and will be given sufficient time (five minutes instead of one minute per case) to review the images and produce an actionable report. The new format allows for more complex plain radiographs to be included in the exam, across a variety of clinical scenarios, and with multiple pathologies.
This was the subject of extensive and wide-ranging discussion by members of the Project Board and key stakeholders. There were several reasons why the decision was made that the Short Cases would include only abnormal cases. Some of the factors considered are listed below:
- The existing Rapid Reporting does not fully assess a candidate’s ability to identify significant pathology or their ability to compose a concise and accurate report with relevant management advice. Consultant radiologists now have less exposure to plain radiographic reporting during training but will be expected to answer queries from junior radiologists or reporting radiographers for challenging cases throughout their career. Core competence in plain radiograph reporting therefore needs to undergo thorough assessment as part of the exam to ensure that trainees are motivated to master this important component of departmental workload.
- It is unrealistic to ask a candidate to decide whether a case is ‘normal’ or ‘abnormal’ in the absence of relevant clinical history or information about the source of the referral (e.g. general practice versus emergency department). Training radiologists are well aware that, for example, a ‘normal’ chest radiograph does not exclude an underlying lung cancer and that a normal appendicular radiograph does not exclude a fracture in the appropriate clinical setting, so may be reluctant to call a case normal in the absence of clinical information.
- Access to CT and MRI has increased since the Rapid Reporting component was introduced, so radiologists now have the freedom to use these modalities in the appropriate clinical setting where a plain radiograph appears normal.
- It is more difficult to create a fair mark scheme for a normal case with appropriate weighting within the structure of the exam without unwittingly demonstrating to the candidate which cases are normal. Abnormal cases included in the exam all contain numerous normal anatomical structures and, as such, will also test a candidate’s ability to recognise normality.
- Exclusion of normal cases allows the candidate to be assessed on a greater range of pathological conditions, thus making the assessment more robust.
Short, simple statements of your observations, diagnosis and recommendation are all that is needed. You do not need to write full sentences. Sample exam content will be available on the website soon.
Examiners will have access to question-specific marking schemes for each case.
The Oral component is marked by the pair of examiners conducting each session. Scores from all examiners (across both stations) are then totalled.
All Short Case and Long Case questions are independently double marked and scores from both examiners contribute to your total final score.
See the scoring system for more details.
We are not changing exam fees because of these changes.
All candidates will receive a pass/fail notification with a breakdown of their scores across the three components.
From June 2025 all candidates will be assessed using the new format, regardless of any previous attempts.
The type of content used in the exam is unchanged and the same minimum standards for passing the exam apply. Previous exam attempts will still count.
All candidates are advised to familiarise themselves with the new elements of the exam so that you know what to expect during the exam.