June 2025 FRCR Part 2B (Radiology) - CR2B - scoring system
LEARN MOREPlease note details referenced below will be applicable from the June 2025 exam diet onwards. CR2B exams prior to this will continue to be delivered in the current scoring system format.
Context
The FRCR Part 2B Exam consists of three scoring components: an Oral assessment; Long Case reporting and Short Case reporting. Established and recognised standard setting methodologies (Angoff and Ebel) are used to determine the pass mark for the exam. Each component will have its own standard set pass mark and candidates must reach the standard across all three components in order to achieve an overall pass at the exam (with some allowance for borderline scores – see section on overall scoring). It is not possible to carry forward a pass in any one component from a previous sitting. If an overall fail result is awarded, candidates must re-sit the entire exam.
Oral component
Candidates are assessed across two 30-minute Oral stations. At each station candidates will be presented with six cases. There are two examiners present at each station and each case will be independently marked by both examiners. All cases are assessed across the four following skill domains:
- Radiology knowledge
- Observation
- Clinical reasoning
- Clinical safety and management.
Each examiner will rate a candidate’s performance for each of the domains per case using the following rating scale:
| Score | Marking descriptors |
| Excellent | Display positive domain characteristics at a level well above that expected. |
| Clear pass | Display of positive domain characteristics is predominant overall. Some minor negative characteristics are displayed. Competence is clearly demonstrated. |
| Just pass | Display of positive domain characteristic is predominant by a small margin. Should be able to provide some of the positive characteristics without the need for prompting, i.e. not require prompting for all of them. Some negative characteristics are displayed but they are not in the majority or decisive with a potential to be dangerous or harmful to patients. A minimum level of competence is achieved. |
| Borderline fail | No predominance of positive or negative domain characteristics displayed. Negative characteristics displayed not potentially harmful to patients. A barely adequate level of competence is achieved. |
| Fail | Display a majority of negative domain characteristics. Negative domain characteristics displayed are potentially harmful to patients. The required level of competence is not achieved. |
Communication domain
Additionally, at each station examiners will assess the communication domain. This is a rating based on performance across all six cases in the station. Candidates are rated using the same rating scale as above.
Example of a candidate’s scoring for one station from one examiner:
|
CASE |
Knowledge |
Observation |
Clinical reasoning |
Clinical safety and management |
|
1 |
E |
CP |
JP |
BF |
|
2 |
JP |
JP |
JP |
F |
|
3 |
E |
CP |
JP |
B |
|
4 |
CP |
CP |
BF |
BF |
|
5 |
CP |
E |
CP |
CP |
|
6 |
JP |
CP |
CP |
JP |
|
Communication |
CP |
|||
After the exam, all ratings are converted to numerical format (0-4) as follows:
Excellent (E) = 4
Clear pass (CP) = 3
Just pass (JP) = 2
Borderline fail (BF) = 1
Fail (F) = 0
As the communication score is assessed per station, it is multiplied by six to ensure it has the same weighting as the other four skill domains.
Scores from all examiners (across both stations) are then totalled to give the candidate’s total score (out of a maximum of 480). The marking framework permits a difference of up to five marks between the two examiners per case. Any score difference of six or above per case will be flagged for review and discussion.
The pass mark of 281 (58.5%) has been determined via the Ebel/Angoff standard setting methodology. This is applied to the candidate’s total score to determine their pass/fail outcome for the Oral exam.
Long Case reporting
Candidates report on six cases and have the opportunity to attain five marks for each case, so a maximum of 30 marks across the exam. No half marks are awarded. Candidate responses are independently double marked and the final score awarded will be the average of the two examiner marks. The marking framework permits a difference of up to one mark between the two examiners. Any score difference of two or above will be flagged for review and discussion.
All questions include question specific marking guidance to indicate key findings, diagnosis and recommended onward management. Examiners will use the following mark scheme descriptors alongside the marking guidance to support mark allocation:
| Score | Marking descriptors |
| 5 |
Detects all major findings and most minor observations. Makes correct diagnosis or differential diagnoses using clinical information provided. Makes safe further management plans with clear recommendations (including MDT or specialist referral if appropriate). Demonstrates a clear understanding of likely further management required by different MDTs. Report is clear, logical and concise. May demonstrate knowledge beyond the core curriculum. |
| 4 |
Detects most major findings (including those marked essential) and most minor observations. Makes correct diagnosis or differential diagnoses using clinical information provided. Makes safe further management plans with clear recommendations (including MDT or specialist referral if appropriate). Report is clear, logical and concise. |
| 3 |
Detects most major findings (including those marked essential) and some minor observations. May or may not reach the correct diagnosis but demonstrates sensible clinical reasoning. Safe differential diagnoses offered. May not know full management plan but demonstrates enough knowledge not to compromise patient safety. Report is clear although it may not be ideally structured |
| 2 |
Fails to detect most major/critical (essential) observations. Fails to make correct diagnosis or provide reasonable differential diagnoses. Inappropriate further management or failure to refer to appropriate MDT. Unstructured, scattergun report. |
| 1 |
Fails to detect major observations or places undue importance on minor or incidental observations. Makes an incorrect or inappropriate diagnosis, failing to consider clinical information. Incoherent, rambling report. |
| 0 |
No answer provided or answer is entirely incorrect or inappropriate/unsafe patient management. |
An Angoff standard setting process is used to set the pass mark for each sitting based on the content used.
Short Case reporting
Candidates report on 25 cases and have the opportunity to attain five marks per case, so a maximum of 125 marks across the exam. No half marks will be allocated. Candidate responses are independently double marked and the final score awarded will be the average of the two examiner marks. The marking framework permits a difference of up to one mark between the two examiners. Any score difference of two or above will be flagged for review and discussion.
All questions include question-specific marking guidance to indicate key findings, diagnosis and recommended onward management. Examiners will use the following mark scheme descriptors for examiners alongside the marking guidance to score candidates’ responses:
| Score | Marking descriptors |
| 5 |
Detects all major findings and most minor observations. Makes correct diagnosis or differential diagnoses using clinical information provided. Makes safe further management plans with clear recommendations (including MDT or specialist referral if appropriate). Demonstrates a clear understanding of likely further management required by different MDTs. Report is clear, logical and concise. May demonstrate knowledge beyond the core curriculum.
|
| 4 |
Detects most major findings (including those marked essential) and most minor observations. Makes correct diagnosis or differential diagnoses using clinical information provided. Makes safe further management plans with clear recommendations (including MDT or specialist referral if appropriate). Report is clear, logical and concise.
|
| 3 |
Detects most major findings (including those marked essential) and some minor observations. May or may not reach the correct diagnosis but demonstrates sensible clinical reasoning. Safe differential diagnoses offered. May not know full management plan but demonstrates enough knowledge not to compromise patient safety. Report is clear although it may not be ideally structured. |
| 2 |
Major/critical observations missed. Undue significance placed on irrelevant or minor findings. Limited understanding of pathology. Fails to make correct diagnosis or provide reasonable differential diagnoses. Failure to refer to appropriate MDT/clinical team or inappropriate over-investigation e.g. MRI and orthopaedic referral for benign bone lesions. Unstructured, scattergun report.
|
| 1 |
Major/critical observations missed. Undue significance placed on minor or incidental findings Inappropriate patient management (including over-investigation). Incoherent, rambling report. |
| 0 |
No answer provided or answer is entirely incorrect or inappropriate/unsafe patient management. |
An Angoff standard setting process is used to set the pass mark for each sitting based on the content used.
Short case reporting sample questions
Sample short cases and sample answers are provided below to give guidance on what constitutes a good, average and poor answer. Short, simple statements of your observations, diagnosis and recommendation are all that is needed. You do not need to write full sentences.
The examiner marking guidance shown next to the sample answers is intended to give context on the marking of each case. The examiner marking guidance indicates key findings, diagnosis and recommended onward management to help to explain why a particular answer would score more than another. Examiners will use the mark scheme descriptors (as detailed in the scoring system) alongside this marking guidance to score candidates’ responses and each case will be awarded a score of 0 – 5. There is no concept of a pass or fail per case as all cases are standard set as to their difficulty. The modified Angoff process is used to determine the pass mark for each sitting based on the content used.
Please note that the examiner marking guidance will not be available to candidates as part of their results/feedback.
Age 14, male. Referral from ED. History: Painful wrist after falling off skateboard.

| Sample answer | Answer type | Examiner marking guidance |
|
Distal radius fracture through the growth plate, with dorsal displacement. |
Good |
Age 14, male. Referral from ED. History: Painful wrist after falling off skateboard. Findings: Management: |
|
There is a displaced fracture of the distal radius with dorsal displacement (Colles type fracture). |
Average |
|
|
Left radiocarpal dislocation |
Poor |
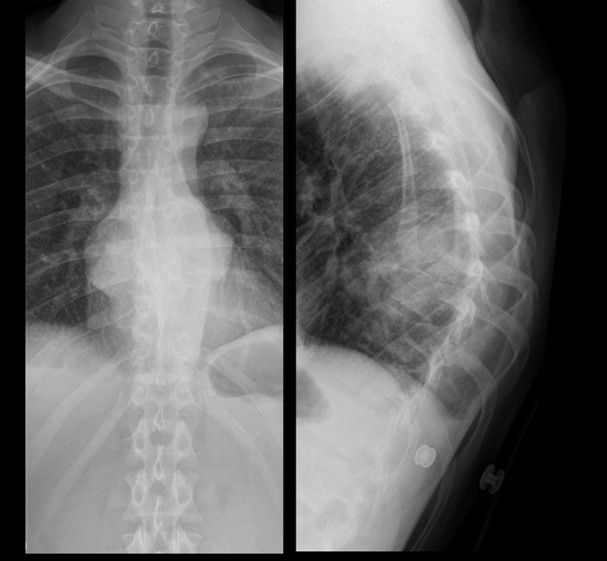
Age 81 male. Referral from GP. History: Cough and weight loss

| Sample answer | Answer type | Examiner marking guidance |
|
Triangular opacity projected over the left heart with obscuration of the medial left hemidiaphragm and loss of volume of the left hemithorax. Increased density noted at the left hilum. Appearances are in keeping with left lower lobe collapse. Causes include central obstructing tumour and mucus plugging. Lungs show multiple confluent opacities some showing appearance in keeping with pleural plaques (I would compare with previous studies). There is prominent right paratracheal soft tissue. Urgent CT chest and upper abdomen to further investigate. |
Good |
Age 81 male. Referral from GP. History: Cough and weight loss Findings: |
|
Left lower lobe collapse with volume loss CT thorax, abdomen and pelvis for further evaluation and staging |
Average |
|
|
Right upper zone mediastinal mass medially likely posterior mediastinum, apical/parenchymal mass cannot be excluded. Bilateral ill-defined patchy focal lesions and reticular opacities. |
Poor |
Age 18 female. Referral from GP. History: painful left knee

| Sample answer | Answer type | Examiner marking guidance |
|
There is an osteochondral defect in the lateral aspect of the medial femoral condyle. There is a bone fragment centrally within the joint space. No joint effusion. Knee MRI and Orthopaedic referral |
Good |
Age 18 female. Referral from GP. History: painful left knee Findings:
|
|
There is lucency projected over the lateral femoral condyle of left femur in keeping with an osteochondral defect. A cortical fragment seen in the intercondylar space. No large knee joint effusion identified. Normal alignment Orthopaedic referral and further assessment with MRI may prove beneficial. |
Average |
|
|
Well-defined lesion in the right distal femur, with sclerotic margins and a narrow zone of transition. No periosteal bone formation. Referral to orthopaedics due to pain. No concerning imaging features so no further investigation needed. |
Poor |
Age 31 male. Referral from ED. History: Post assault

| Sample answer | Answer type | Examiner marking guidance |
|
Right angle of the mandible fracture Refer to max fax surgeon for further management |
Age 31 male. Referral from ED. History: Post assault
Findings: |
|
|
Acute fracture of the right mandibular angle Formal OPG/mandibular views to assess for further fracture. |
Average |
|
|
Left inferior orbital rim fracture Referral to maxillofacial surgeons |
Poor |
New-born male. Referral from NNU. History: traumatic birth due to shoulder dystocia, query clavicular fracture.

| Sample answer | Answer type | Examiner marking guidance |
|
-Nasogastric tube passes into stomach, tip not visualised. Urgently phone NNU to ensure findings are known.
|
Good |
New-born male. Referral from NNU. History: traumatic birth due to shoulder dystocia, query clavicular fracture Findings: |
|
Patient rotated to the left. Notify NICU team.
|
Average |
|
|
NGT in situ appears satisfactory. no clavicle fracture or dislocation seen. imaged lungs appear normal. No further management |
Poor |
Age 24 male. Referral from GP. History: increasing back pain
| Sample answer | Answer type | Examiner marking guidance |
|
Bilateral paravertebral stripe widening at T8 with collapse of T8 vertebral body and kyphosis. Urgent MRI whole spine with contrast. Inform referrer urgently. Antibiotics. Microbiology. Drainage. |
Good |
Age 24 male. Referral from GP. History: increasing back pain Findings: |
|
Soft tissue mass in the posterior mediastinum causing complete collapse and destruction of a mid-thoracic vertebra and focal kyphosis, this is concerning for spondylodiscitis Compare to previous CXR, email GP the report, advise urgent MRI spine for further evaluation |
Average |
|
|
-Paravertebral soft tissue densities projected in the retrocardiac region bilaterally. This corresponds with density projected over vertebral bodies on the lateral projection Imp: Paravertebral masses - likely neurogenic e.g. Neurofibroma, schwannoma MRI Thorax is advised. |
Poor |
Overall scoring
In order to pass the exam, candidates must meet the established pass mark in at least two of the three exam components. Candidates who fail two or more of the three exam components automatically fail overall. Candidates who pass all of the three exam components automatically pass overall.
For candidates who have met the pass mark for two of the three exam components, a pass overall is given provided that the following additional criteria are met:
- If the candidate has failed either the Long Case reporting OR Short Case reporting but met the pass mark for the Oral and for one reporting component, they will pass overall if they have scored within one standard error of measurement (SEm) below the pass mark for the failed exam component.
- If the candidate has failed the Oral exam but met the pass mark in both the Long Case reporting and Short Case reporting exam components, they will pass overall if they have scored within half a SEm below the pass mark for the Oral exam.
The standard error of measurement (SEm) is calculated using the exam’s reliability and standard deviation. It gives an estimate of how much a candidate’s observed score (the score they actually achieved in the exam) might vary from their true score. A 'true score' is the theoretical or 'real' level of a candidate's ability or knowledge, free from any statistical measurement error that could affect the exam score. The SEm shows the range within which the true score is likely to lie, providing a measure of precision around the observed score.
The Gold Award
The Gold Award can be awarded to an outstanding candidate on recommendation of the Exam Board, based on performance, at each sitting of the exam.
To be considered for the Award, a candidate must be making their first attempt at the exam and have obtained the highest score overall. In the event of a tie, the candidate with the highest scores in the Oral component will be the recipient of the Award.
Our exams
Find out more about our FRCR exams in clinical radiology and clinical oncology, and DDMFR exams in dental and maxillofacial radiology.
